Ulcers are wounds or sores that do not heal or take a long time to heal. They can occur on any part of the body, but leg ulcers are a common problem. Leg ulcers are usually the result of poor blood flow to the legs, leading to tissue damage and ulceration. Arterial leg ulcers and venous leg ulcers are two different types of leg ulcers caused by different underlying conditions. In this blog Dr. Sumit Kapadia, Senior Varicose Vein Specialist and Vascular Surgeon, will discuss the differences between arterial leg ulcers and venous leg ulcers, their symptoms, causes, and treatment.
What is Arterial Leg Ulcer?
Arterial leg ulcers are caused by poor blood circulation in the arteries that supply the legs. The arteries are responsible for carrying oxygen-rich blood from the heart to the legs. When there is a blockage in the arteries, the blood supply to the legs is reduced, leading to tissue damage and ulceration.
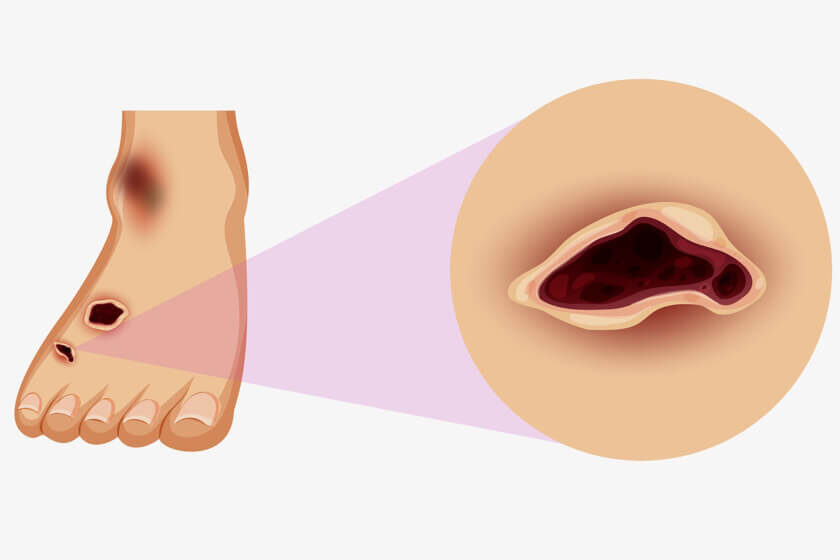
Symptoms of Arterial Ulcer
Arterial leg ulcers typically appear on the feet and lower legs. They are usually small, round, and deep, with a defined edge. The skin around the ulcer may be shiny, dry, and discolored. The ulcer may be painful, especially when the leg is elevated. In severe cases, the ulcer may be surrounded by blackened or necrotic tissue ( also popularly called as gangrene). Arterial leg ulcers are caused by poor blood flow in the arteries that supply the legs. This poor blood flow can lead to tissue damage and the development of a non-healing sore, which can eventually become an ulcer. The symptoms of arterial leg ulcers may include:
Pain:
Arterial ulcers can be very painful, especially when the leg is elevated or the person is lying down. The pain is often described as a sharp, burning, or throbbing sensation. This pain at rest may sometimes cause difficulty in sleeping.
Skin changes:
The skin around the ulcer may be pale, shiny, dry, or cool to the touch. The area may also be discolored, such as red, blue, or purple.
Non-healing sore:
The ulcer may be open and weeping, with a yellow or brownish crust. It may be surrounded by a red, purple or blackish border.
Slow healing:
Arterial ulcers are slow to heal, and may not respond to traditional wound care methods.
Infection:
If left untreated, arterial ulcers can become infected, leading to increased pain, redness, swelling, and fever.
Gangrene:
In severe cases, the lack of blood flow to the affected area can lead to tissue death, or gangrene. This is one of the most common causes requiring major amputation below or even above the knee.
It is important to seek medical attention from a varicose vein specialist & Vascular Surgeon if you have any symptoms of an arterial leg ulcer. Early diagnosis and treatment can prevent complications and improve the chances of successful healing.
Also read: Veins vs. Arteries: What’s the Difference?
What is Venous Leg Ulcer?
Venous leg ulcers are caused by poor blood circulation in the veins that drain blood from the legs. The veins are responsible for carrying deoxygenated or impure blood from the legs back to the heart. When the veins are damaged or weakened, blood can pool in the legs, leading to tissue damage and ulceration.
Symptoms of Venous Ulcers
Venous leg ulcers typically appear on the lower leg, around the ankle or on the inside of the leg. They are usually larger and shallow compared to arterial leg ulcers, with an irregular shape and poorly defined edge. The skin around the ulcer may be swollen, red, and itchy, and may weep or ooze fluid. The ulcer may be painful, especially when the leg is dependent or when walking. Venous leg ulcers are caused by poor blood flow in the veins that drain blood from the legs. This poor blood flow can lead to tissue damage and the development of a non-healing sore, which can eventually become an ulcer. The symptoms of venous leg ulcers may include:
Swelling:
The affected leg may be swollen, especially around the ankle and lower leg. The swelling may be accompanied by a feeling of heaviness or aching.
Skin changes:
The skin around the ulcer may be discolored, such as red, brown, or purple. The skin may also be thickened, dry, or scaly. These changes are often irreversible and called lipodermatosclerosis in medical language.
Non-healing sore:
The ulcer may be open and weeping, with a yellow or greenish discharge. It may be surrounded by a red or purple border, and there may be small blood vessels visible on the surface.
Itching:
The skin around the ulcer may be itchy, which can make the area more difficult to tolerate.
Pain:
Venous ulcers may be painful, especially if they become infected or are located in a sensitive area.
Infection:
If left untreated, venous ulcers can become infected, leading to increased pain, redness, swelling, and fever.
It is important to seek medical attention from Varicose Vein Specialist & Vascular Surgeon if you have any symptoms of a venous leg ulcer. Early diagnosis and treatment can prevent complications and improve the chances of successful healing.
Causes of Arterial leg ulcers and venous leg ulcers
Arterial leg ulcers and venous leg ulcers are caused by different underlying conditions.
Arterial leg ulcers are caused by poor blood flow in the arteries that supply the legs. This poor blood flow is usually due to atherosclerosis or peripheral artery disease, which are conditions that cause narrowing and hardening of the arteries. Other risk factors for arterial leg ulcers include smoking, diabetes, high blood pressure, and high cholesterol levels.
Venous leg ulcers are caused by poor blood flow in the veins that drain blood from the legs. This poor blood flow is usually due to venous insufficiency, which is a condition that causes damage to the valves in the veins, leading to pooling of blood and increased pressure in the veins. This can be seen in patients who have varicose veins or deep vein thrombosis. Other risk factors for venous leg ulcers include obesity, pregnancy, and a history of deep vein thrombosis.
In both cases, the poor blood flow leads to tissue damage and a non-healing sore, which can eventually become an ulcer. Without proper treatment, the ulcer can become infected and lead to further complications. It is important to see a healthcare professional if you have any symptoms of a leg ulcer to receive a proper diagnosis and treatment.
Arterial Ulcers Vs Venous Ulcers
Arterial and venous leg ulcers are caused by different underlying conditions, and their symptoms and treatment options vary accordingly. Here are some of the key differences between arterial and venous leg ulcers:
Location:
Arterial leg ulcers typically occur on the feet and lower legs, while venous leg ulcers are more common on the lower leg and ankle.
Size and shape:
Arterial ulcers are usually small, round, and deep, with a defined edge. Venous ulcers are larger, shallow, and irregular in shape, with a poorly defined edge.
Pain:
Arterial ulcers are often painful, especially when the leg is elevated. Venous ulcers may be painful or itchy, especially when the leg is dependent or when walking.
Skin changes:
Arterial ulcers are usually surrounded by dry, shiny, and discolored skin. Venous ulcers are surrounded by swollen, red, and itchy skin that may weep or ooze fluid.
Underlying condition:
Arterial leg ulcers are caused by poor blood flow in the arteries, which can be due to atherosclerosis, peripheral artery disease, or other conditions that affect the arterial circulation. Venous leg ulcers are caused by poor blood flow in the veins, which can be due to venous insufficiency, deep vein thrombosis, or other conditions that affect the venous circulation.
Arterial Leg Ulcer Treatment
The primary goal of treating arterial leg ulcers is to improve blood flow to the affected area. This may involve treating the underlying condition that is causing the poor blood flow, such as atherosclerosis or peripheral artery disease. Treatment options may include:
Medications:
Depending on the underlying condition, medications such as blood thinners, cholesterol-lowering drugs, or medications to improve blood flow may be prescribed.
Lifestyle changes:
Quitting smoking, eating a healthy diet, and increasing physical activity can help improve arterial circulation.
Wound care:
Cleaning and dressing the ulcer, debridement (removal of dead tissue), and compression therapy can help promote healing.
Angioplasty:
For adequate wound healing, restoration of blood flow is essential and can be achieved by minimally invasive endovascular techniques like leg vessel Angioplasty done by expert Vascular & Endovascular Surgeons.
Surgery:
In severe cases, surgery may be needed to bypass or remove the blocked or damaged arteries.
Also read: Varicose Veins Laser Treatment Cost In India
Venous Leg Ulcer Treatment
The primary goal of treating venous leg ulcers is to improve blood flow and reduce swelling in the affected area. This may involve treating the underlying condition that is causing the poor blood flow, such as venous insufficiency or deep vein thrombosis. Treatment options may include:
Compression therapy:
This involves wearing compression stockings or bandages to reduce swelling and improve blood flow. We use specialised 3 or 4 layered bandages to help in ulcer healing.
Surgery:
In some cases, surgery may be needed to cover the large ulcers by skin grafting.
Laser or Sclerotherapy:
Patients with ulcers due to varicose veins will often benefit and show faster healing when the root cause of varicose veins is treated by minimally invasive techniques like Laser or sclerotherapy.
Medications:
Depending on the underlying condition, medications such as blood thinners or antibiotics may be prescribed.
Wound care:
Cleaning and dressing the ulcer, debridement, and other wound care techniques can help promote healing.
Conclusion
Arterial and venous leg ulcers are two different types of leg ulcers caused by different underlying conditions. Arterial leg ulcers are caused by poor blood flow in the arteries that supply the legs, while venous leg ulcers are caused by poor blood flow in the veins that drain blood from the legs. The symptoms, location, size, and shape of these ulcers differ as well. The treatment options depend on the underlying condition and may include lifestyle changes, medications, wound care, and surgery.
If you have any symptoms of a leg ulcer, such as a non-healing sore, it is important to see a Varicose Vein Specialist & Vascular surgeon for an evaluation. Early diagnosis and treatment can help prevent complications and improve the chances of successful healing.
Follow us on YouTube

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.