What’s the Connection Between Peripheral Artery Disease, Diabetes, and Gangrene?
A middle-aged man walked into my clinic with a limp and a worried look on his face. He spoke of persistent pain in his leg and a slow-healing wound on his foot. A diabetic for over a decade, he’d grown accustomed to minor discomforts. But this time, it was different. The pain was sharp, the wound darkened ominously, and walking had become an ordeal. It was clear he needed immediate medical attention. What followed was a discussion about the Diabetes and Gangrene connection, as we explored the Diabetes and Gangrene connection and how it worsened his condition. We also discussed the underlying issues caused by Diabetes and Gangrene connection and the importance of timely intervention. This led to further insights into the critical aspects of the Diabetes and Gangrene connection and its potential consequences if left untreated.
What is Peripheral Artery Disease (PAD)?
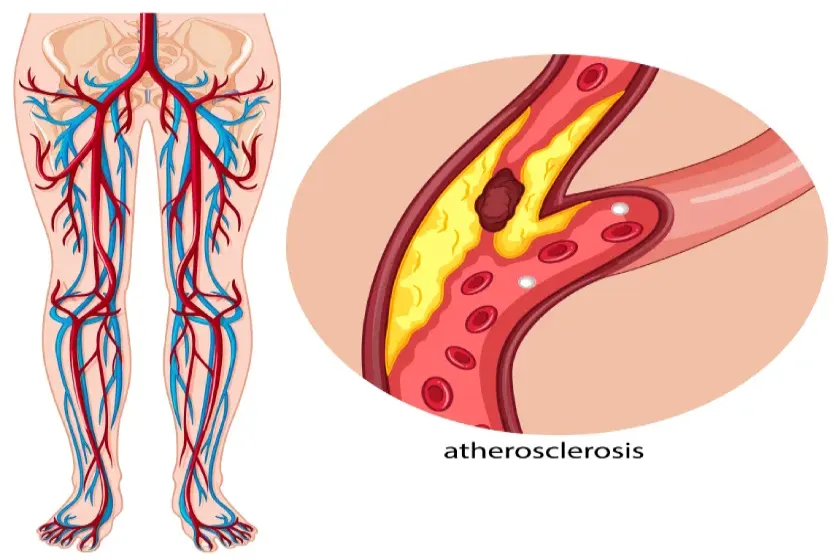
Peripheral Artery Disease (PAD) is a circulatory condition caused by the narrowing or blockage of arteries, typically in the legs, due to plaque buildup. This restricts blood flow to the extremities, leading to symptoms such as pain while walking (claudication), numbness, or slow-healing sores. In India, an estimated 10% to 20% of individuals above the age of 60 suffer from PAD, often undiagnosed until severe complications arise.
PAD is not merely a condition of inconvenience; it’s a warning sign of widespread vascular issues, increasing the risk of heart attacks and strokes. If left untreated, the reduced blood supply can lead to tissue death, setting the stage for gangrene.
Diabetes and Its Impact on Blood Circulation
Diabetes is a known culprit for wreaking havoc on blood vessels. Chronically high blood sugar levels damage blood vessels and nerves, impairing circulation, especially to the lower limbs. According to the International Diabetes Federation, over 74 million Indians are living with diabetes, many of whom are at risk of developing PAD.
For diabetic patients, poor circulation is compounded by peripheral neuropathy—a condition where nerves lose their ability to sense pain. This often delays the detection of injuries or ulcers, which can worsen into severe infections and, eventually, gangrene.
Understanding Gangrene
Gangrene refers to the death of body tissue caused by a lack of blood flow or a severe bacterial infection. It classically manifests as a black-colored patch. It most commonly affects the extremities, including the feet and toes. There are two main types:
- Dry Gangrene: Occurs due to a lack of blood supply and is marked by shriveled, blackened tissue.
- Wet Gangrene: Associated with bacterial infections, leading to swollen, pus-filled tissue. Wet gangrene can rapidly spread and become life-threatening if not treated promptly.
In diabetics and those with PAD, gangrene is not just a possibility—it’s a looming threat.
The Connection Between PAD, Diabetes, and Gangrene
The trio of PAD, diabetes, and gangrene forms a dangerous cycle. Here’s how they interlink:
- Diabetes accelerates atherosclerosis (plaque buildup in arteries), which causes PAD.
- PAD restricts blood flow, making it harder for wounds or infections to heal.
- Poor healing creates an ideal environment for gangrene to develop.
The statistics are stark: 30% of diabetic foot ulcers progress to gangrene if left untreated, and gangrene is a leading cause of lower-limb amputations in India. Early diagnosis of PAD and diabetes management can significantly reduce these risks.
Early Signs to Watch For
Early detection is crucial in preventing severe complications. Look out for the following symptoms:
PAD Symptoms:
- Leg pain or cramping while walking (claudication)
- Coldness or numbness in the lower limbs
- Slow-healing sores or ulcers
- Discoloration of the skin on the legs
Gangrene Symptoms:
- Persistent pain or swelling in the affected area
- Skin that turns red, purple, or black
- Foul-smelling discharge
- Loss of sensation in the affected region
If you experience any of these signs, consult a vascular specialist immediately.
Preventive Measures
Preventing PAD, diabetes complications, and gangrene involves proactive measures:
- Control Blood Sugar: Keep diabetes well-managed through regular monitoring, medications, and a healthy diet.
- Maintain Healthy Cholesterol Levels: Reduce plaque buildup by avoiding high-fat diets and ensuring regular exercise.
- Quit Smoking: Smoking exacerbates arterial damage and accelerates PAD.
- Inspect Your Feet Daily: Check for cuts, sores, or discoloration, especially if you have diabetes.
- Wear Proper Footwear: Avoid tight or ill-fitting shoes that can cause injuries.
- Routine Checkups: Regular visits to a vascular specialist can help in the early detection of PAD and other complications.
Treatment Options
The treatment of PAD and gangrene depends on the severity of the condition:
- Lifestyle Changes: Diet, exercise, and smoking cessation can slow disease progression.
- Medications: Blood thinners, cholesterol-lowering drugs, and medications to improve blood flow are commonly prescribed.
- Endovascular Treatment: Minimally invasive procedures such as angioplasty or stenting can restore blood flow.
- Surgical Interventions: In severe cases, bypass surgery may be needed to reroute blood around blocked arteries.
- Amputation: If gangrene is advanced and cannot be controlled, amputation may be the only option to save the patient’s life
When to Consult a Specialist
If you have diabetes or symptoms of PAD, consulting a vascular specialist is vital. Delaying treatment can lead to irreversible complications, including gangrene and potential limb loss.
In Vadodara, Dr. Sumit Kapadia, a renowned vascular surgeon, specializes in diagnosing and treating PAD, diabetic complications, and gangrene. With advanced diagnostic tools and a patient-centric approach, he’s helped countless patients regain their mobility and improve their quality of life.
Conclusion
The connection between Peripheral Artery Disease, diabetes, and gangrene underscores the importance of vigilance and timely medical intervention. Managing diabetes, recognizing early signs of PAD, and seeking prompt treatment can prevent devastating outcomes like gangrene and limb amputation.
Remember, your health is in your hands. Regular checkups, a healthy lifestyle, and expert guidance from a vascular specialist like Dr. Sumit Kapadia can help you lead a life free from the crippling effects of PAD and gangrene. Don’t wait for a minor issue to escalate—act today to safeguard your tomorrow.
FAQ
PAD is a condition where arteries become narrowed due to plaque buildup, reducing blood flow to the extremities. This leads to symptoms like pain, numbness, and slow-healing wounds.
Diabetes damages blood vessels and nerves, impairing circulation and delaying wound healing, which can lead to infections and gangrene.
Early signs include skin discoloration, persistent pain, foul-smelling discharge, and numbness in the affected area.
Yes, with proper diabetes management, early detection of PAD, and timely medical intervention, the risk of gangrene can be minimized.
Treatment includes lifestyle changes, medications, endovascular procedures, and in severe cases, surgery or amputation.
Consult a specialist if you experience symptoms like leg pain, slow-healing wounds, or discoloration of the skin. Early diagnosis is key to preventing complications.
Maintain good blood sugar control, avoid smoking, inspect your feet daily, and have regular checkups with a vascular specialist.



