Understanding Diabetic Ulcers
In India, where diabetes is a growing concern, understanding diabetic foot problems and ulcers is crucial. Dr Sumit Kapadia, a prominent figure in diabetic wound care, shares valuable insights into this condition that affects a significant portion of the diabetic population. This comprehensive guide covers everything from causes and symptoms to advanced treatment options and effective management strategies.
Definition
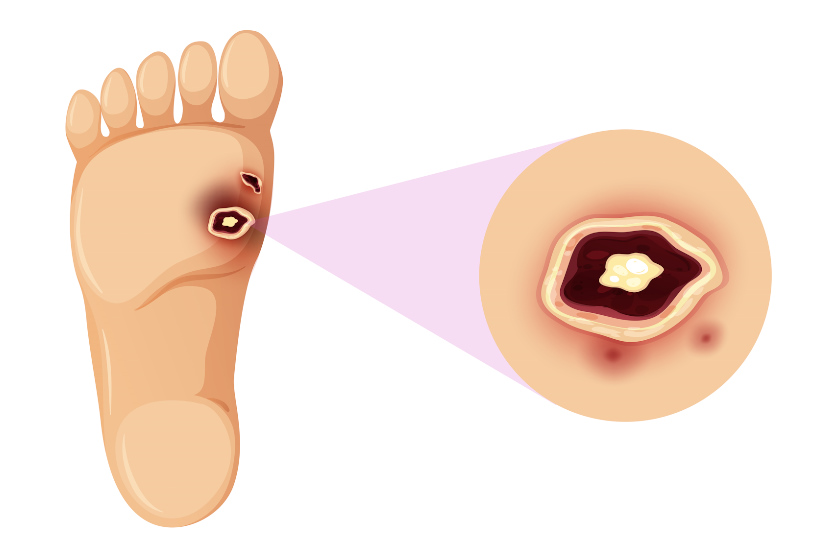
Diabetic ulcers are open sores or wounds, typically on the foot, that occur in individuals with diabetes. These ulcers stem from a combination of factors including neuropathy (nerve damage), poor blood circulation, and high blood sugar levels, making healing difficult and leading to severe complications if not managed effectively.
Types of Diabetic Ulcers
Diabetic ulcers are a significant complication for individuals with diabetes. Understanding the different types can help in identifying and treating these wounds more effectively. Here’s a closer look at each type:
Neuropathic Ulcers:
Characteristics: These ulcers occur primarily in patients who have lost the ability to feel pain due to diabetic neuropathy. As a result, they may not notice small injuries, leading to the development of ulcers.
Common Locations: Typically found on pressure points of the foot like the ball, heel, or under the big toe.
Appearance: They often have a well-defined edge and are surrounded by thick skin and callosity.
Ischemic Ulcers:
Characteristics: Caused by poor blood circulation and lack of oxygen supply due to arterial disease. These ulcers are more common in patients with peripheral artery disease (PAD).
Common Locations: Found in areas of the feet and legs where blood flow is restricted, such as the toes and lower legs.
Appearance: They tend to be deeper and more painful, with a pale or bluish colouration around the wound. These may aggravate over time and lead to gangrene.
Neuro-ischemic Ulcers:
Characteristics: A combination of both neuropathy and poor circulation, these ulcers are more complex and difficult to treat.
Common Locations: Can appear in similar areas as neuropathic and ischemic ulcers.
Appearance: They may combine the characteristics of both neuropathic and ischemic ulcers.
Causes of Diabetic Ulcers
Understanding the causes of diabetic ulcers is crucial in their prevention and management. The primary causes include:
High Blood Sugar Levels:
Effect: Prolonged high blood sugar levels can lead to damage in the nerves (neuropathy) and blood vessels, affecting the blood flow and sensation in the legs and feet.
Result: This damage makes it difficult for even minor wounds to heal, increasing the risk of ulcers.
Neuropathy (Nerve Damage):
Effect: Neuropathy reduces the ability to feel pain or notice injuries on the feet.
Result: Minor injuries such as cuts or blisters can go unnoticed and worsen over time, developing into ulcers.
Poor Circulation:
Effect: Diabetes can lead to narrowed arteries, reducing blood flow to the feet.
Result: Reduced blood flow means wounds heal slowly or not at all, leading to ulcer formation.
Foot Deformities and Pressure Points:
Effect: Diabetes can cause changes in the feet, like bone deformities or dry skin, leading to pressure points and increased risk of skin breakdown.
Result: Continuous pressure on certain parts of the foot can lead to skin breakdown and ulcer formation.
Inadequate Footwear:
Effect: Shoes that don’t fit well can cause rubbing or pressure.
Result: This constant pressure can lead to skin damage and eventually ulcers.
Trauma or Injury:
Effect: Even minor injuries can lead to ulcers in diabetic individuals due to the compromised healing process.
Result: Cuts, scrapes, or other foot injuries can escalate into serious ulcers if not treated promptly.
Infections:
Effect: Diabetic individuals are more prone to infections, which can complicate or lead to the development of ulcers.
Result: Infections can quickly escalate, turning minor wounds into serious ulcers.
By understanding these types and causes, patients with diabetes and healthcare providers, like Dr Sumit Kapadia, can work together more effectively to prevent and treat diabetic ulcers. Regular foot examinations, proper diabetic management, and immediate attention to foot injuries are key to preventing the development of these ulcers.
Symptoms of Diabetic Ulcers
Diabetic ulcers, particularly concerning for those with diabetes, can develop without significant pain due to nerve damage. Being vigilant about the following symptoms is crucial:
Visible Sores or Wounds:
Significance: A noticeable sore or wound on the foot, especially on pressure points such as the heel or ball of the foot.
Appearance: These sores can range from superficial to deep, exposing underlying tissues.
Swelling Around the Wound:
Indication: Swelling or puffiness near a wound or on the foot can be an early sign of an ulcer or an infection.
Redness and Warmth:
Significance: Red, warm skin around a wound suggests inflammation and possibly an underlying infection.
Drainage from the Wound:
Observation: Unusual discharge or fluid seeping from a wound on the foot. This might stain socks or leak inside shoes.
Foul Odor:
Concern: A bad smell emanating from a foot wound is often an indication of infection.
Black Tissue Around the Wound:
Explanation: Known as eschar, black tissue surrounding a wound indicates tissue death and can be a sign of a severe ulcer.
Pain or Tingling:
While many with diabetic ulcers might not experience pain, some might feel tingling or a dull ache around the ulcer site.
Diagnosis of Diabetic Ulcers
Early and accurate diagnosis of diabetic ulcers is vital for effective treatment. The process typically includes:
Physical Examination:
A thorough inspection of the feet for any wounds, sores, or signs of infection. Special attention is given to areas under the toes and the soles of the feet.
Medical History Review:
Understanding the patient’s history of diabetes, including blood sugar control, neuropathy, previous foot problems, and lifestyle habits.
Neuropathy Assessment:
Testing for loss of sensation in the feet using monofilament testing or tuning forks. This helps to determine the presence and extent of neuropathy. There are also special Neuroscan machines available for this purpose.
Blood Flow Examination:
Checking the pulses in the feet and legs to assess blood circulation. Poor blood flow can impede healing and increase the risk of ulcers. An Ankle Brachial Index ( ABI or ABPI) is often used as a screening test in diabetic patients to detect slower blood flow.
Imaging Tests:
X-rays, MRI, or CT scans may be used to view the bones and tissues in the foot, especially if an infection is suspected to have spread to the bone (osteomyelitis).
Wound Culture:
If infection is suspected, a sample from the ulcer may be taken to identify the type of bacteria present, guiding antibiotic therapy.
Blood Tests:
To check for signs of infection or other conditions that might affect healing, such as elevated blood sugar levels or kidney problems.
Understanding the symptoms and undergoing proper diagnosis procedures are crucial steps in managing diabetic ulcers. Regular foot inspections and immediate attention to any abnormalities can significantly improve outcomes. Dr. Sumit Kapadia emphasizes the importance of early detection and comprehensive diabetic foot care to prevent the progression of these ulcers. By incorporating effective diabetic ulcer management strategies, individuals with diabetes can maintain better foot health and avoid complications associated with these ulcers.
Complications of Diabetic Ulcers
Diabetic ulcers, if not properly managed, can lead to severe complications. These complications are particularly concerning due to the compromised healing ability in individuals with diabetes. Here’s a detailed look at the possible complications:
Infections:
Diabetic ulcers can easily become infected due to their open nature and slower healing process. Infections can range from mild to severe, potentially involving the deeper tissues or bones (osteomyelitis). Infections can exacerbate the ulcer, making it more difficult to heal and increasing the risk of systemic complications. In some patients, these infections can spread very fast from the foot to the leg within a few days.
Gangrene:
Gangrene refers to the death of body tissue due to a lack of blood flow or a severe bacterial infection. It’s a serious condition that can lead to amputation if not treated promptly. The affected area may turn black and emit a foul odour.
Amputation:
In severe cases, where the ulcer or infection does not respond to treatment, amputation of the toe, foot, or part of the leg may be necessary. Regular monitoring and early treatment of diabetic ulcers are crucial in preventing this drastic measure.
Charcot Foot:
A condition where the bones in the foot become weakened due to nerve damage and can fracture or dislocate, leading to deformities. t’s a serious complication that can develop if a diabetic ulcer leads to significant nerve damage and poor blood flow.
Prevention of Diabetic Ulcers
Prevention is key when it comes to diabetic ulcers. Here are some effective strategies to prevent these ulcers:
Regular Foot Inspections:
Daily checking of feet for cuts, blisters, red spots, and swelling. Using a mirror can help inspect hard-to-see areas.
Proper Foot Care:
Keeping feet clean and dry, moisturizing to prevent cracks, trimming toenails carefully, and avoiding walking barefoot to prevent injuries.
Blood Sugar Control:
Maintaining blood sugar levels within the target range as advised by a healthcare provider helps in preventing complications of diabetes, including foot ulcers.
Wearing Appropriate Footwear:
Using well-fitting, comfortable shoes that provide good support and cushioning. Special diabetic shoes are also available that minimize pressure points and reduce the risk of skin breakdown.
Regular Medical Check-Ups:
Regular visits to a healthcare provider for comprehensive foot exams can help in the early identification of potential problems.
Smoking Cessation:
Smoking worsens blood circulation, heightening the risk of ulcers and other complications. Quitting smoking can significantly improve circulation.
Managing Other Health Conditions:
Keeping conditions like hypertension and cholesterol under control, as they can contribute to circulation problems, increasing the risk of ulcers.
Patient Education:
Dr. Sumit Kapadia’s Emphasis: Educating patients about the importance of foot care, recognizing early signs of foot problems, and seeking prompt medical attention is crucial. Knowledge about diabetic wound care and ulcer prevention is vital.
By following these preventive measures, individuals with diabetes can significantly reduce their risk of developing foot ulcers. Dr. Sumit Kapadia advocates for a proactive approach to managing diabetes and its complications, emphasizing the importance of patient awareness and regular care in preventing diabetic ulcers.
Treatment of Diabetic Ulcers with Dr. Sumit Kapadia
Treatment of diabetic ulcers requires a multifaceted approach that addresses both the wound and the underlying causes. Dr. Sumit Kapadia, a renowned expert in diabetic wound care, offers a range of treatment options:
Wound Care:
Cleaning and Dressing: Regular cleaning and appropriate dressing of the ulcer to prevent infection and promote healing. We use and recommend a wide variety of special dressing materials for helping in ulcer healing.
Debridement: Removal of dead tissue from the ulcer to encourage the growth of healthy tissue.
Medication Management:
Antibiotics: To treat and prevent infection.
Pain Management: Medications to alleviate pain associated with the ulcer.
Advanced Treatment Options:
Offloading: Using devices like special footwear, casts, or braces to relieve pressure on the ulcer.
Negative Pressure Wound Therapy (NPWT): Promotes healing by applying suction to the wound.
Advanced Wound healing : We use advanced methods like Stimulan, Matriderm, Integra or Polynova BTM to improve granulation and reduce infections. These methods are especially useful in larger ulcers or ulcers which do not heal with basic treatment.
Surgical Interventions:
Vascular Surgery: Procedures to improve blood flow to the affected area, especially in cases of ischemic ulcers. Most diabetic patients would have multi level arterial blockages or blockages in smaller blood vessels below the knee and hence experienced and expert vascular surgeons can do angioplasty or distal bypasses to improve the blood flow to the foot and help in ulcer healing.
Skin Grafts: In severe cases, skin grafts may be used to cover large or deep ulcers.
Lifestyle Modifications:
Diet and Exercise: Customized advice on diet and exercise to manage diabetes effectively.
Foot Care Education: Guidance on daily foot care to prevent future ulcers.
Regular Monitoring and Follow-up:
Continuous Assessment: Regular check-ups to monitor the healing process and adjust treatments as necessary.
Management and Lifestyle Recommendations for Diabetic Ulcers
Managing diabetic ulcers effectively involves more than just medical treatment; it requires adopting a comprehensive lifestyle approach that addresses the root causes and prevents recurrence. Here’s a detailed look at lifestyle and management strategies:
Balanced Diet:
Nutrition: Focus on a diet rich in vegetables, whole grains, lean proteins, and fruits. Limit intake of processed foods, high sugar, and unhealthy fats.
Blood Sugar Control: Consistent monitoring and maintaining a diet that helps keep blood sugar levels stable.
Regular Physical Activity:
Exercise Benefits: Regular exercise improves blood circulation, helps in weight management, and aids in controlling blood sugar levels.
Recommended Activities: Low-impact exercises like walking, swimming, or cycling are beneficial. However, it’s important to wear appropriate footwear and avoid activities that might cause foot injuries.
Foot Hygiene and Care:
Daily Inspection: Check feet daily for any signs of cuts, blisters, or injuries. Seek immediate medical attention for any signs of infection or non-healing wounds.
Proper Footwear: Wear well-fitting, comfortable shoes that protect the feet. Avoid tight shoes that can cause pressure points.
Smoking Cessation:
Impact of Smoking: Smoking can significantly worsen blood circulation, making it crucial for individuals with diabetes to quit smoking.
Stress Management:
Stress and Blood Sugar: High stress can affect blood sugar levels. Practices like meditation, yoga, or light exercise can help manage stress.
Regular Health Check-ups:
Professional Oversight: Regular visits to a Vascular surgeon or Hospital with having department of vascular surgery for comprehensive diabetes management and foot care are essential. If possible, a complete diabetic foot health checkup which may consist of ABPI, Neuroscan and Podoscan can be performed at 6 monthly or 1 year intervals.
Patient Education:
Awareness: Understanding the risks associated with diabetes and foot care is vital. Dr. Sumit Kapadia emphasizes the importance of patient education in the management of diabetic ulcers.
Under the care of Dr. Sumit Kapadia, patients with diabetic ulcers receive comprehensive treatment that not only addresses the immediate medical needs but also focuses on long-term management and prevention strategies. His approach ensures that patients are well-equipped with the knowledge and tools needed to manage their condition effectively and maintain overall foot health.
Dr Sumit Kapadia’s Approach to Diabetic Ulcers
As an expert in diabetic wound care, Dr Sumit Kapadia emphasizes a multidisciplinary approach to the effective management of diabetic ulcers. His treatment protocol includes:
Advanced Wound Care Techniques: Utilizing the latest in wound dressing materials and technologies.
Patient Education and Engagement: Ensuring patients understand their condition and the importance of foot care.
Collaborative Care: Working alongside diabetes specialists, nutritionists, and podiatrists for comprehensive patient care.
Conclusion
Diabetic ulcers require vigilant care and management to prevent severe complications. With the right approach to treatment and lifestyle modifications, it’s possible to effectively manage these ulcers. Dr Sumit Kapadia’s comprehensive care in this field stands as a beacon of hope for those suffering from this challenging complication of diabetes. For more information or to schedule a consultation, patients are encouraged to reach out to Dr. Sumit Kapadia’s team.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.



