Comprehensive Guide to Peripheral Angioplasty
Peripheral angioplasty stands as a significant advancement in the field of vascular medicine, offering a promising solution to individuals grappling with peripheral artery disease (PAD) and related vascular conditions.
Conducted by top vascular surgeons in India and worldwide, this minimally invasive procedure holds the potential to alleviate symptoms and improve blood circulation in the limbs, particularly the legs. Despite its remarkable efficacy, peripheral angioplasty can evoke apprehension due to concerns about the procedure itself, recovery, and associated costs.
In this comprehensive guide, we aim to shed light on peripheral angioplasty, unraveling its procedural nuances, objectives, and potential benefits. By addressing concerns such as peripheral angioplasty cost and post-operative care, our goal is to empower individuals to approach their vascular health journey with confidence and informed decision-making.
What is Peripheral Angioplasty and How Does It Work?
Peripheral angioplasty is a minimally invasive surgical procedure used to treat peripheral artery disease (PAD), a condition characterized by the narrowing or blockage of arteries in the limbs, most commonly the legs. This narrowing, often caused by the buildup of plaque or fatty deposits within the artery walls, can lead to decreased blood flow to the affected limb, resulting in symptoms such as leg pain, cramping, numbness, and weakness.
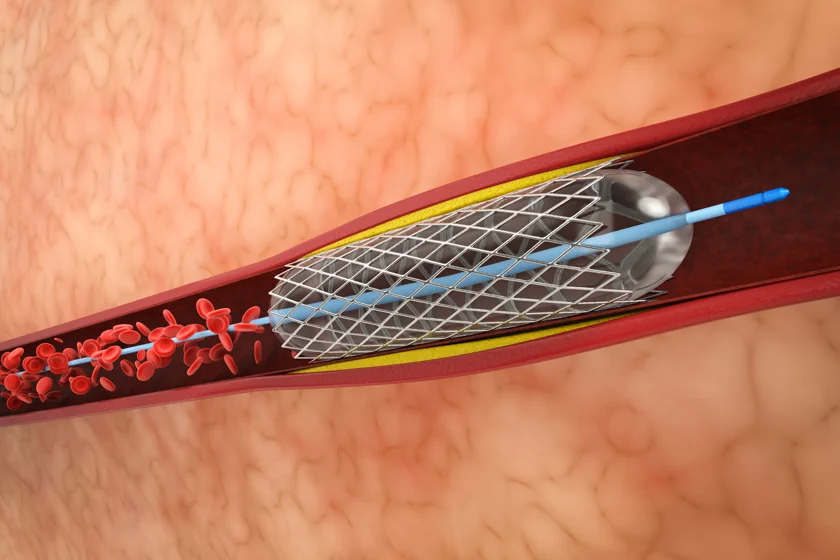
During peripheral angioplasty, a highly trained vascular surgeon guides a catheter, a thin, flexible tube, into the affected artery through a small incision, typically in the groin area. The catheter is then advanced to the site of the blockage or narrowing using fluoroscopic guidance, a real-time X-ray imaging technique. Once the catheter reaches the target area, a deflated balloon attached to its tip is positioned within the narrowed portion of the artery.
Next, the balloon is carefully inflated, exerting outward pressure on the plaque or fatty deposits and compressing them against the walls of the artery. This process widens the narrowed passage, restoring proper blood flow to the downstream tissues and improving circulation to the affected limb. In some cases, a stent, a small mesh-like tube, may be inserted into the newly widened artery to help keep it open and prevent re-narrowing, a process known as restenosis.
Peripheral angioplasty is typically performed under local anesthesia, meaning the patient remains awake but may receive medication to relax or sedate them. This minimally invasive approach offers several advantages over traditional open surgeries, including shorter recovery times, reduced risk of complications, and avoidance of large surgical incisions.
Following the procedure, patients are typically monitored for a short period in a recovery area before being discharged home on the same day or the following day. While some patients may experience mild discomfort or bruising at the incision site, most can resume normal activities within a few days to weeks, depending on individual factors and the extent of the procedure.
Overall, peripheral angioplasty represents a significant advancement in the treatment of PAD, offering patients a safe, effective, and minimally invasive option to improve blood flow to the limbs and alleviate symptoms associated with vascular disease.
Purpose of Peripheral Angioplasty
The primary purpose of peripheral angioplasty is to improve blood circulation in the limbs, particularly the legs, by addressing blockages or narrowing in the peripheral arteries. This minimally invasive procedure is used to treat peripheral artery disease (PAD) and other vascular conditions that restrict blood flow to the extremities.
By widening narrowed or blocked arteries through the inflation of a balloon catheter, peripheral angioplasty restores proper blood flow to the affected limb, alleviating symptoms such as leg pain, cramping, numbness, and weakness. This improvement in blood circulation not only enhances mobility and quality of life but also reduces the risk of complications associated with compromised blood flow, such as tissue damage, ulcers, and limb amputation.
In addition to symptom relief, peripheral angioplasty can help prevent the progression of peripheral artery disease, reducing the likelihood of further arterial blockages and the need for more invasive treatments such as bypass surgery or amputation. Moreover, by restoring blood flow to the affected limb, peripheral angioplasty promotes wound healing and improves overall vascular health, contributing to better long-term outcomes for patients with PAD.
Overall, the purpose of peripheral angioplasty is to provide a safe, effective, and minimally invasive solution for individuals suffering from peripheral artery disease, allowing them to regain mobility, independence, and quality of life while minimizing the risk of complications associated with vascular disease.
Common Risks Associated with Peripheral Angioplasty
While peripheral angioplasty is generally considered safe and effective, like any medical procedure, it carries certain risks and potential complications. Some of the common risks associated with peripheral angioplasty include:
Bleeding: Bleeding at the catheter insertion site is common, especially if the patient is taking blood-thinning medications or has a bleeding disorder. In most cases, this bleeding is minor and resolves on its own, but in rare cases, it may require medical intervention.
Arterial Damage: There is a risk of injury to the artery during the insertion of the catheter or inflation of the balloon, which could lead to bleeding, hematoma formation, or arterial dissection (tearing of the artery wall).
Blood Clots: The manipulation of the artery during angioplasty can dislodge plaque or other debris, which may travel downstream and cause a blood clot (embolism). This can potentially block blood flow to a smaller artery and lead to tissue damage or other complications.
Restenosis: Despite the initial success of the procedure, there is a risk of the treated artery becoming narrowed again (restenosis) over time. This can occur due to scar tissue formation or the recurrence of plaque buildup within the artery.
Infection: While rare, there is a risk of infection at the catheter insertion site or within the bloodstream (sepsis) following angioplasty. Proper sterile technique during the procedure and careful post-operative wound care can help minimize this risk.
Allergic Reaction: Some patients may experience an allergic reaction to the contrast dye used during the procedure, which can cause symptoms such as rash, itching, or difficulty breathing. This risk is higher in patients with a known allergy to iodine or contrast dye.
Kidney Damage: The contrast dye used during angioplasty can potentially cause kidney damage, especially in patients with pre-existing kidney disease or dehydration. Adequate hydration before and after the procedure can help reduce this risk.
Stroke: In rare cases, the manipulation of the catheter within the arteries can dislodge plaque or other debris, which may travel to the brain and cause a stroke. This risk is higher in patients with pre-existing cerebrovascular disease or severe arterial blockages in the neck arteries.
Also read- Understanding the Link Between Carotid Artery Disease and Stroke
Factors Influencing the Success of Peripheral Angioplasty
Several factors can influence the success of peripheral angioplasty, including:
Extent and Location of Arterial Blockage: The severity and location of the arterial blockage play a significant role in determining the success of angioplasty. Blockages that are shorter and located in larger arteries are generally more amenable to treatment with angioplasty.
Patient’s Overall Health: The patient’s overall health and medical history, including the presence of other medical conditions such as diabetes, hypertension, and kidney disease, can impact the success of angioplasty. Patients with well-controlled medical conditions generally have better outcomes.
Arterial Anatomy: The size, tortuosity, and accessibility of the affected artery can affect the ease of performing angioplasty and the likelihood of achieving a successful outcome. Complex arterial anatomy may require additional expertise or specialized equipment.
Operator Experience: The experience and skill of the vascular surgeon performing the angioplasty are crucial factors in determining the procedure’s success. Experienced operators are better equipped to navigate challenging anatomy, minimize complications, and achieve optimal results.
Technical Factors: Various technical factors, such as the choice of balloon size, inflation pressure, and duration, as well as the use of adjunctive devices like atherectomy or stenting, can influence the success of angioplasty. Proper technique and equipment selection are essential for achieving optimal outcomes.
Patient Compliance: Patient compliance with pre-and post-operative instructions, including medication adherence, lifestyle modifications, and follow-up appointments, can impact the long-term success of angioplasty. Compliance with recommended treatments and lifestyle changes is crucial for maintaining arterial patency and preventing the recurrence of arterial blockages.
Complications: The occurrence of procedural complications, such as arterial dissection, perforation, or embolization, can influence the success of angioplasty. Prompt recognition and management of complications are essential for minimizing adverse outcomes and optimizing procedural success.
Post-procedural Care: Adequate post-procedural care, including monitoring for complications, optimizing medical therapy, and implementing lifestyle modifications, is critical for maintaining the benefits of angioplasty and preventing the recurrence of arterial blockages.
Conclusion
In conclusion, the success of peripheral angioplasty hinges on a multitude of factors, ranging from patient-specific variables to technical expertise and post-procedural care. By carefully considering these factors and tailoring treatment plans to individual patient needs, vascular surgeons like Dr. Sumit Kapadia can optimize the likelihood of achieving favorable outcomes with peripheral angioplasty.
Dr. Sumit Kapadia emphasizes the importance of a comprehensive approach to peripheral angioplasty, encompassing thorough patient evaluation, meticulous procedural technique, and attentive post-operative care. Through his expertise and dedication to excellence, Dr. Kapadia strives to deliver superior outcomes and improve the vascular health and quality of life of his patients.
In partnering with Dr. Sumit Kapadia, patients can trust in his unwavering commitment to their well-being and confidence in his ability to deliver exceptional results through peripheral angioplasty and other cutting-edge vascular treatments.
FAQs
Recovery from peripheral angioplasty typically takes a few days to a week. Most patients can resume normal activities within a few days, although strenuous activities may need to be avoided for a bit longer.
Peripheral angioplasty is generally not painful, as it is performed under local anesthesia. Some patients may experience mild discomfort or soreness at the catheter insertion site, but this usually resolves quickly.
The cost of peripheral angioplasty can vary depending on factors such as the location, the healthcare facility, the complexity of the procedure, and any additional treatments or services required. But one can expect to shed around Rs. 40,000 to Rs. 70,000 for the surgery.
Yes, most patients can walk shortly after leg angioplasty. The procedure is aimed at improving blood flow to the legs, which can alleviate symptoms and enhance mobility.
The number of arterial blockages that can be successfully treated with angioplasty depends on various factors, including the location, size, and severity of the blockages, as well as the patient’s overall health and vascular anatomy. In some cases, multiple blockages can be addressed during a single angioplasty procedure, while in others, additional treatments may be necessary to address all blockages.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.



