Although earlier believed to be a western disease, almost all Vascular & Endovascular surgeons in India have seen the numbers of Indians affected by this disease increasing over the past 2 decades. According to a popular study by the SAGE group, peripheral arterial disease would probably affect 40 to 50 million Indian citizens, out of which 4 to 6 million would suffer from a severe form of PAD called critical limb ischemia (CLI).
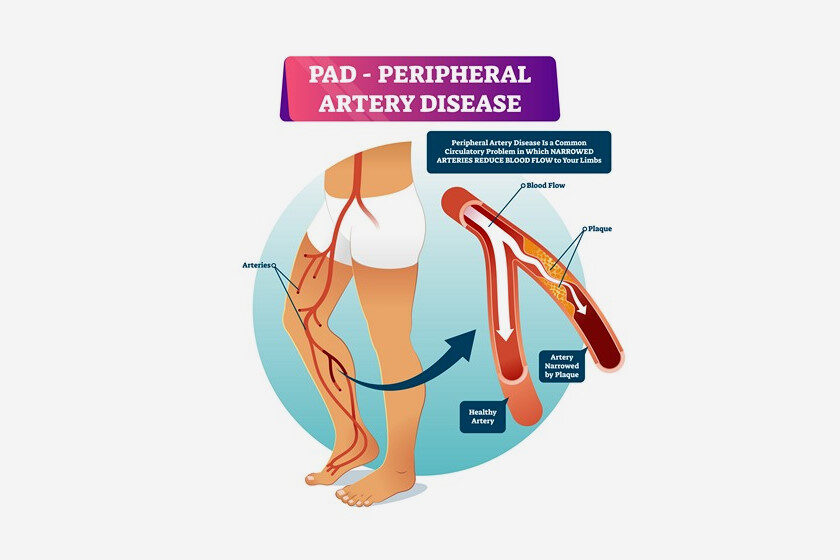
Peripheral vascular disease (PVD) or peripheral arterial disease (PAD) is blockage of arteries of the lower limbs due to accumulation of cholesterol, calcium and plaques. This leads to reduced blood and oxygen supply to the legs and may eventually lead to limb amputations as well as suffering due to rest pain and gangrene. Most of the causative factors are similar to that for heart diseases, but the awareness level for peripheral arterial disease is very less as compared to that for heart blockages.
Here are 5 important things one should know about PAD
- Early PAD may not have noticeable symptoms. Symptoms may not be noticeable in early stages as symptoms do not develop till there is significant reduction in blood flow to the legs. The classic symptom of claudication (pain in muscles on walking for a fixed distance) also may not be noted if the affected person is not walking longer distances. Some people may often disregard these early symptoms as old age or muscle weakness. A proper evaluation by a vascular surgeon would be helpful in identifying this problem in the early stages.
- PAD is a high-risk factor for heart disease. If you have PAD, there is a high chance of atherosclerosis or blockage of heart arteries. Studies have shown that 30 to 40% of all patients with PAD will have some evidence of heart disease. Additionally, another 10 to 15% will have carotid artery disease, often leading to stroke and paralysis. Hence, patients suffering from PAD during its treatment may occasionally end up with heart attacks or stroke.
- Advanced PAD can lead to amputation. Untreated and advanced PAD can progress and lead to critical limb ischemia in which the blood flow to legs is so critically impaired that it causes severe pain at rest along with ulcers or gangrene. At this stage, conservative treatment methods usually are not very effective and these patients would need an immediate or early interventional or surgical treatment. Many of these patients with advanced PAD may ultimately end up with progressive gangrene and require amputation below or above the knee. Also Read: 8 Tips to Improve Blood Circulation in Legs & Feet
- PAD can be treated conservatively. Most patients with early detected PAD can be managed conservatively by medical treatment (antiplatelets like aspirin, statins and Cilostazol) along with lifestyle changes and walking exercises. The control of risk factors like Diabetes, Hypertension (high Blood Pressure), smoking cessation and control of cholesterol levels is of paramount importance to prevent worsening of the disease. Consult our vascular surgeon in time to know if your PAD can be treated conservatively. There are no vascular physicians in our country at present. So a trained Vascular & Endovascular surgeon would be the best specialist to guide about which treatment method would be most suitable for your problem.
- Advanced PAD can often be treated without surgery. Minimally invasive endovascular techniques through needle punctures and utilizing low profile balloons or stents have revolutionized the treatment of PAD patients. There have been substantial developments in the skills and resources utilized for endovascular procedures over the past decade. Continuously upgrading expertise has led to development of drug coated balloons, atherectomy devices and vascular mimetic stents which are proven to deliver better results. Hence more than 70 % of patients with advanced PAD or critical limb ischemia are now treated with angioplasty with the advantages of rapid recovery and faster relief of symptoms.
Our vascular and endovascular specialists can guide you and help provide a suitable balanced option between the different available procedures based on multiple factors including age, co-existent problems, level of blockages and availability or expense of devices.
Think Vascular Think Aadicura
Follow us on YouTube

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.

MBBS, MS, MRCS, DNB-Fellow
Dr. Sumit Kapadia
Dr. Sumit Kapadia / MR KAPADIA SUMIT a gold-medalist from Baroda Medical College, obtained his general surgical training and senior residency from SSG Hospital, Vadodara.